Cutting off a brain enzyme reversed Alzheimer’s plaques in mice
Knocking back an enzyme swept mouse brains clean of protein globs that are a sign of Alzheimer’s disease. Reducing the enzyme is known to keep these nerve-damaging plaques from forming. But the disappearance of existing plaques was unexpected, researchers report online February 14 in the Journal of Experimental Medicine.
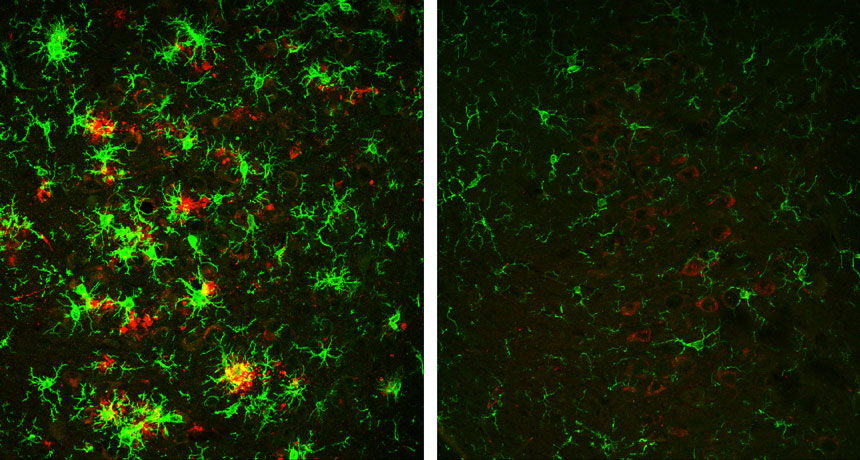
The brains of mice engineered to develop Alzheimer’s disease were riddled with these plaques, clumps of amyloid-beta protein fragments, by the time the animals were 10 months old. But the brains of 10-month-old Alzheimer’s mice that had a severely reduced amount of an enzyme called BACE1 were essentially clear of new and old plaques.
Studies rarely demonstrate the removal of existing plaques, says neuroscientist John Cirrito of Washington University in St. Louis who was not involved in the study. “It suggests there is something special about BACE1,” he says, but exactly what that might be remains unclear.
Story continues below graphic
One theory to how Alzheimer’s develops is called the amyloid cascade hypothesis. Accumulation of globs of A-beta protein bits, the idea goes, drives the nerve cell loss and dementia seen in the disease, which an estimated 5.5 million Americans had in 2017. If the theory is right, then targeting the BACE1 enzyme, which cuts up another protein to make A-beta, may help patients.
BACE1 was discovered about 20 years ago. Initial studies turned off the gene that makes BACE1 in mice for their entire lives, and those animals produced almost no A-beta. In humans, however, any drug that combats Alzheimer’s by going after the enzyme would be given to adults. So Riqiang Yan, one of the discoverers of BACE1 and a neuroscientist at the Cleveland Clinic, and colleagues set out to learn what happens when mice who start life with normal amounts of BACE1 lose much of the enzyme later on.
The researchers studied mice engineered to develop plaques in their brains when the animals are about 10 weeks old. Some of these mice were also engineered so that levels of the BACE1 enzyme, which is mostly found in the brain, gradually tapered off over time. When these mice were 4 months old, the animals had lost about 80 percent of the enzyme.
Alzheimer’s mice with normal BACE1 levels experienced a steady increase in plaques, clearly seen in samples of their brains. In Alzheimer’s mice without BACE1, however, the clumps followed a different trajectory. The number of plaques initially grew, but by the time the mice were around 6 months old, those plaques had mostly disappeared. And by 10 months, “we hardly see any,” Yan says.
Cirrito was surprised that getting rid of BACE1 later in life didn’t just stop plaques from forming, but removed them, too. “It is possible that perhaps a therapeutic agent targeting BACE1 in humans might have a similar effect,” he says.
Drugs that target BACE1 are already in development. But the enzyme has other jobs in the brain, such as potentially affecting the ability of nerve cells to communicate properly. It may be necessary for a drug to inhibit some, but not all, of the enzyme, enough to prevent plaque formation but also preserve normal signaling between nerve cells, Yan says.