Nanoparticles beat back atherosclerosis
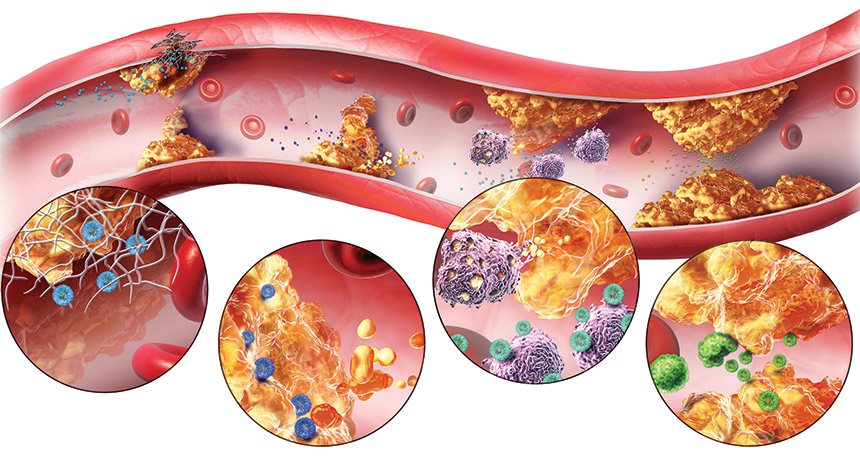
Careening through the bloodstream, a single nanoparticle is dwarfed by red blood cells whizzing by that are 100 times larger. But when specially designed nanoparticles bump into an atherosclerotic plaque — a fatty clog narrowing a blood vessel — the tiny particles can play an outsized role. They can cling to the plaque and begin to break it down, clearing the path for those big blood cells to flow more easily and calming the angry inflammation in the vicinity.
By finding and busting apart plaques in the arteries, nanoparticles may offer a new, non-surgical way to reduce a patient’s risk for heart attack and stroke.
Nanoparticles measure less than 100 nanometers across — a thousandth the thickness of a dollar bill. Despite being tiny, they can be engineered to haul a mix of molecules — such as tags that make them stick to a plaque, drugs that block inflammation or dyes that let scientists track their movements. Over the last two decades, scientists have exploited these strategies to fight cancer, designing nanoparticles that deliver drugs (SN Online: 1/3/14) or dyes for imaging deep into the core of a tumor. The U.S. Food and Drug Administration has approved a few dozen cancer-focused nanomedicines.
Now researchers have begun engineering nanoparticles to target cardiovascular disease, which kills even more people each year than cancer. Nanosized compounds have been built that can sweep into clogged arteries to shrink the plaques that threaten to block blood flow. Some nanoparticles home in on the plaques by binding to immune cells in the area, some do so by mimicking natural cholesterol molecules and others search for collagen exposed in damaged vessel walls. Once at the location of a plaque, either the nanoparticles themselves or a piggybacked drug can do the cleanup work.
The aim of all these approaches is to prevent strokes and heart attacks in people with cardiovascular disease, either before surgery becomes necessary or after surgery to prevent a second event. Today, cardiovascular nanoparticles are still far from pharmacy shelves. Most have not reached safety testing in patients. But in mice, rats and pigs, nanodrugs have slowed the growth of the plaques that build up on vessel walls, and in some cases have been able to shrink or clear them.
“I think the effect we can have with these nanoparticles on cardiovascular disease is even more pronounced and direct than what we’ve seen in cancer,” says Prabhas Moghe, a biomedical engineer at Rutgers University in Piscataway, N.J.
Every minute, more than a gallon of blood pumps through the human heart, pushing through miles of blood vessels to deliver oxygen and nutrients to organs and extremities. In a healthy person, the trip is as smooth as a drive on a freshly paved highway. But in the more than 10 percent of U.S. adults who have cardiovascular disease, the route might be more like a pothole-filled road squeezed by Jersey barriers.
Waxy globs, or plaques, of fat and cholesterol line the blood vessels, thickening and hardening the walls, impeding blood flow. As fat builds up inside the vessels, it also leaks into the vessel walls, swelling them and signaling the body to send immune cells to the area. The congregation of immune cells aggravates the blockage, the way emergency vehicles surrounding the site of a multi-car pileup further slow traffic on a highway.
“The inflammation and the accumulation of fat in the walls of the blood vessel sort of feed off each other and exacerbate each other,” Moghe says.
If the plaques grow large enough, or pieces chip off and travel to smaller vessels, they can block a vessel. If oxygen-filled blood can’t reach the brain or heart, a stroke or heart attack results.
The drugs most often prescribed to prevent or treat atherosclerosis — plaque buildup on the inner walls of the arteries — are statins (SN: 5/5/12, p. 30). This highly successful and effective class of drugs, available since 1987, slows the growth of the fatty plaques by lowering the amount of cholesterol circulating in the blood. But taking statins is akin to limiting the number of cars on a damaged road rather than repairing potholes, some argue. And the drugs can boost a person’s risk of diabetes and liver damage. In many cases, patients don’t begin taking statins until they already have severe atherosclerosis, and the drugs do little to reverse the buildup of plaques that already exist.
“Heart disease is still the number one killer in the U.S.,” says endocrinologist and biochemist Ira Tabas of Columbia University Medical Center. Drug-carrying nanoparticles that can shrink existing atherosclerotic plaques and eliminate the accompanying inflammation could change that, Tabas and others say.
Going places
To treat atherosclerotic plaques with nanoparticles, researchers have devised a variety of ways to send circulating particles directly to the fatty clogs. In each approach below, a molecule that’s part of the nanoparticle binds to a molecule in or near the plaques.
Click the black dots in the interactive image below to learn about different types of nanoparticles.
Macrophage magnet
To make nanoparticles congregate at the dangerous plaques, researchers need to identify something that makes the blockage stand out from the rest of the body. The crowds of immune cells near plaques act as a signpost that a plaque exists.
Many of the immune cells involved in atherosclerosis are macrophages, white blood cells that gulp pathogens, dead cells or debris in the body. At the site of a plaque, macrophages become swollen with fats and transform into what are called “foam cells” because of their foamy appearance. As they digest fats, foam cells send out chemical signals to recruit more inflammation-causing cells and molecules to the area. Because they’re so intimately involved in the formation of plaques, macrophages and foam cells are a prime target for nanoparticles.
Moghe’s group has designed nanoparticles that bind to molecules on the surface of macrophages, preventing them from gobbling fats and becoming foam cells. The researchers made the nanoparticles specifically target a subtype of macrophage that’s involved in atherosclerosis, not the macro-phages that might respond to other injuries in the body. When nanoparticles were injected into mice with narrowed arteries, the blockages decreased by 37 percent, Moghe’s group reported last year in the Proceedings of the National Academy of Sciences.
Others are using cholesterol-like molecules as nanoparticle taxis to carry drugs to plaques and subdue the immune reaction. Statins aim to lower the form of cholesterol called low-density lipoprotein, which earned the name “bad cholesterol” for accumulating in plaques. High-density lipoprotein, or “good cholesterol,” shuttles LDL away from these clogs to the liver, where it can be broken down. HDL also prevents macro-phages from turning into foam cells and producing inflammatory molecules. So Shanta Dhar, a chemist at the University of Georgia in Athens, developed nanoparticles that mimic HDL. She presented the work in March in San Diego at a meeting of the American Chemical Society.
“HDL is our body’s natural cholesterol-removing nanomaterial,” she says. In animal tests, the HDL-based nanoparticle can bind to free-floating macro-phages circulating in the blood, just as HDL does, and follow them to a plaque, she explains. The nanoparticles can also bind to macrophages already glommed on to a plaque, and, mimicking the activities of natural HDL, carry the cells away.
Plaque buster
Willem Mulder, a nanomedicine researcher at the University of Amsterdam and the Icahn School of Medicine at Mount Sinai in New York City, has also designed HDL-mimicking nanoparticles. His particles deliver statins that make a beeline for macrophages and plaques, letting him administer the drug at lower-than-usual doses. He was inspired by earlier studies that showed how extremely high doses of statins, given to mice, could lower LDL levels while also packing anti-inflammatory properties. Of course, in humans, such high doses would probably cause liver or kidney damage. Mulder’s solution: tack the statins to a nanoparticle to send them, missile-like, to the plaques. That way, a low dose of the drug could achieve the high concentration needed at the site of the atherosclerosis.
“We’re exploiting the inherent targeting properties of HDL,” he says. “And it works well with statins, which are small molecules.”
In 2014 in Nature Communications, Mulder’s group reported that plaque-filled arteries in mice given the nanoparticle were 16 percent more open than arteries in mice with no treatment, and 12 percent more open than in mice given a systemic statin. More work is needed to show whether these modest gains would translate to a reduced risk of heart attacks and strokes.
Others are using plaque-targeting nanoparticles to deliver anti-inflammatory drugs similar to methotrexate, which is used as a treatment for rheumatoid arthritis. The side effects of drugs like this, given systemically, are generally severe: vomiting, hair loss and “brain fog,” to name a few.
“If someone with rheumatoid arthritis comes into your office completely crippled, it’s worth all the side effects to put them on an anti-inflammatory drug,” Tabas says. “But imagine someone with some risk factors for heart disease who feels great. They’re not going to put up with these side effects.”
Tabas thinks that drugs that work distinctly from traditional anti-inflammatory drugs and promote resolution of inflammation and healing, known as pro-resolving drugs, could be perfect candidates to tack on to nanoparticles because they would make possible lower doses with fewer side effects.
He’s awaiting the results of two large clinical trials testing non-nano-versions of the drugs methotrexate and anti-IL1 beta. It remains to be seen whether they’re effective at clearing plaques and how severe the side effect are. If the drugs are effective, even with some side effects, Tabas says, it will give weight to his approach: Activating pro-resolving pathways using targeted nanoparticles.
Tabas and his collaborator Omid Farokhzad at Harvard University encapsulate their nanoparticles with a small section of a protein called annexin A1, which helps resolve inflammation and promote healing. His hope is that delivered only to an atherosclerotic plaque, the drug won’t have the host of side effects that other immune blockers have.
Destination: vessel wall
The inflamed vessel wall around an atherosclerotic plaque goes through several changes in addition to the accumulation of belligerent immune molecules. As vessel walls are stretched and inflamed, the structural protein collagen, meant to keep the vessels taut and tubular, becomes exposed the way the threads of a tire begin to appear as it wears down. Scientists are using the exposed collagen to their advantage. Nanoparticles with a tag recognizing the collagen end up at plaques. But it’s not as easy as affixing a GPS destination to the particles, says vascular surgeon Melina Kibbe of Northwestern University Feinberg School of Medicine in Chicago.
“It took us over a year of trying to find the right targeting [molecule] that would work,” Kibbe says. Her nanoparticle combines a collagen-binding protein with nitric oxide, a molecule that stimulates the growth of new cells at wounds. To maximize the surface area of the drug that contacts the vessel wall, Kibbe’s team arranged the molecules in a line, forming a nanofiber, rather than a sphere. As the fiber is swept through the bloodstream, it binds to exposed collagen, anchoring the nitric oxide in place to spur healing of the artery.
Kibbe and colleagues added fluorescent tags to the nanofibers and showed that the fibers congregated at injured spots on mouse arteries within an hour of injection. The tagged particles remained there for three days and the treated vessels ended up 41 percent more open, the researchers reported in the March Antioxidants & Redox Signaling.
Tabas also uses a collagen-binding protein, one that is organized in a more spherical shape, to get the piece of annexin A1 to atherosclerotic plaques. In mice, the particles stayed in the plaques up to five days after treatment, shrinking the plaque by more than a third, his team reported in Science Translational Medicine in 2015. By comparison, some circulating statins last less than a day in the blood.
Rather than targeting proteins or immune cells, scientists at Harvard’s Wyss Institute for Biologically Inspired Engineering have designed nanoparticles that are activated by the physical squeeze that comes with being swept through a narrowed artery. When the shear force around them increases, a cue that a plaque is present, the nanoparticles release their payload: a clot-dissolving drug called tissue plasminogen activator. The researchers reported late last year in Stroke that the nanoparticle, coupled with a stentlike device placed in the artery, increased the survival rate to more than 80 percent in mice that normally die of a clot entering their lungs.
Pathway to patients
Nanoparticles currently in development for cardio-vascular disease are still in animal testing. While no one has seen major side effects or toxicity in the animal trials so far, it remains a concern with a class of medicines that is so new.
“We sometimes get so wrapped up in exuding only the good stuff about nanomedicine that we forget we also have to look at the side effects,” Dhar says.
Another challenge for atherosclerosis drugs is determining who would benefit from treatment. Kibbe imagines her particles being used first in patients with severe atherosclerosis who receive stents or other invasive procedures to clear their plaques. The procedures are intended to help, she says, “but they actually are so traumatic that they cause injury to the vessel wall.” Due in part to this renewed buildup in the arteries, people who have had one heart attack are at higher risk for a second. Even among people who have a permanent stent put in, which is designed to keep part of an artery clear, up to 20 percent become reblocked. Giving these patients nanoparticle-based drugs could keep them healthy, Kibbe says.
Taken to the next level, nanomedicines “certainly might be able to prevent plaques,” she adds. Tabas imagines his nanoparticles given as a once-a-month injection, but that’s speculation.
Moving to test nanoparticles as a preventive — in the huge percentage of the population at risk for athero-sclerosis — is probably a long way off, Mulder says. According to the U.S. Centers for Disease Control and Prevention, around half of all adult Americans have one of the top risk factors for cardiovascular disease.
“I really don’t foresee that you would start preventively treating patients who don’t have symptoms with nanoparticles,” Mulder says. “But to take a person who’s hospitalized after a heart attack and stick a needle in their arm and infuse nanoparticles, that’s not hard.”
Once a few drugs have been validated as working in clinical trials, researchers expect progress to speed up, since the drug cargo on a nanoparticle engineered to target a plaque could easily be switched out for other drugs. Designing the particles, says Moghe, “is almost like building with pieces of Lego.”
This article appears in the June 11, 2016, issue of Science News with the headline, “Nano for the heart.”
Editor’s Note (revised): This article was edited on July 1 and again on July 2, 2016. Due to a misunderstanding by the writer, a quote in the original article mistakenly implied that researcher Ira Tabas of Columbia University was referring to problems with statins. He was, in fact, referring to problems with anti-inflammatories. He is not a critic of statins. Additional changes were made to clarify the activity of annexin A1. It is not a traditional anti-inflammatory agent, as was stated in the article, but what is called a pro-resolving molecule. Tabas did not develop the nanoparticles he works with, as was implied in the original. We now credit the researcher who developed those nanoparticles.